Original publication by AIMSIB on may 7, 2023
https://www.aimsib.org/2023/05/07/dermatite-seborrheique-origine-et-traitement/
What if we were all wrong about the diagnosis, etiology and treatment of this so common disease, so dramatically «displaying» when it comes to severe forms? Thank you to Bernard Sudan, a Franco-Swiss passionate about clinical research and botany for entrusting us with the results of a lifetime of work around this particular pathology. Seborrheic, not in the least, but curable with perfectly natural means (*), perfectly. Fifty years of career to resist the mockery of corticosteroid manufacturers, it takes courage… Good reading.
History of my research
Since my first publication in 1978 (1) describing my familial atopic dermatitis with tobacco allergen and hapten nicotine, several international observations have confirmed my original work (see history of my work with 64 slides) (2).
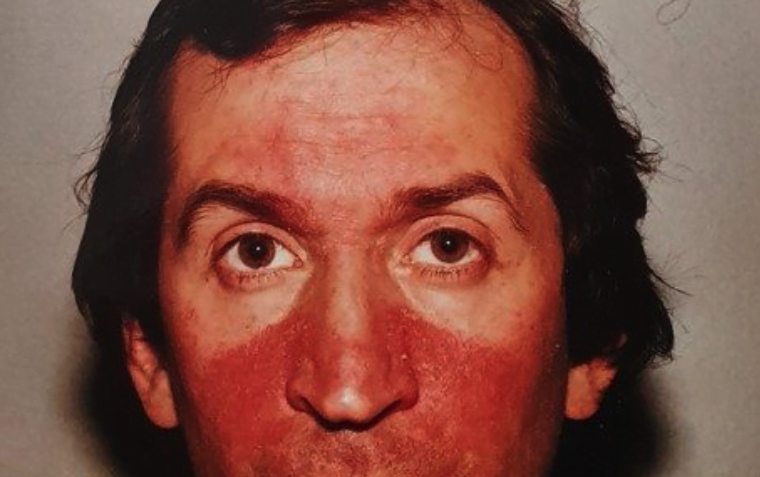
First of all, my familial dermatitis looks like seborrheic facial dermatitis that was first described in 1887.

Sebaceous glands
At the time, dermatologist Unna of Hamburg described eczema as seborrheic because of the presence of many sebaceous glands in this area of the face (3).
Appearance of tobacco smoke
The onset of this dermatological syndrome dates back to a time when tobacco smoke began to invade public places. This seborrheic dermatitis was considered rare in 1903 in a publication of the British Journal of Dermatology (4).
My familial dermatitis
My father had this reaction at about the age of twenty in the early 1930s when he was smoking a few cigarettes. Ten years later, a dermatologist in Belfort prescribed him a very effective solution (2) containing 1/1000 adrenaline with known anti-anaphylactic properties.
At the age of 15, after having solved my asthma, which I had been suffering from for about ten years, and my sudden allergic sinusitis caused by mites, I was surprised to have a reaction to the face with two small red patches on both sides of the nose.
So began my research to elucidate this familial dermatitis that affected my father, my two brothers, my sister and myself. My reactions alternated with phases of desquamation while then finding a normal skin again. The application of corticosteroid creams only worsened this skin reaction.
After I stopped studying medicine, I focused on finding an etiological factor in the environment that causes our family reaction. In addition, my reorientation in a pharmaceutical industry pharmacology and toxicology laboratory in Basel (Switzerland) helped me a lot.
Allergy research
Indeed, I had the chance to conduct an intense bibliographic research in the recent library of the Faculty of Medicine in Basel. I quickly discovered that the German dermatologist Karrenberg (5) caused anaphylactic shock in 1928 after applying a drop of nicotine to 1/1,000,000 in a patient with hand dermatitis, arms and face after handling tobacco leaves. It was then in 1975 and my search accelerated.
Indeed, I had noticed that the proximity of cigar smokers amplified my reactions to the face. In addition, I noticed that my father smoked a cigar on Sundays with also an amplification of his reaction to the face.
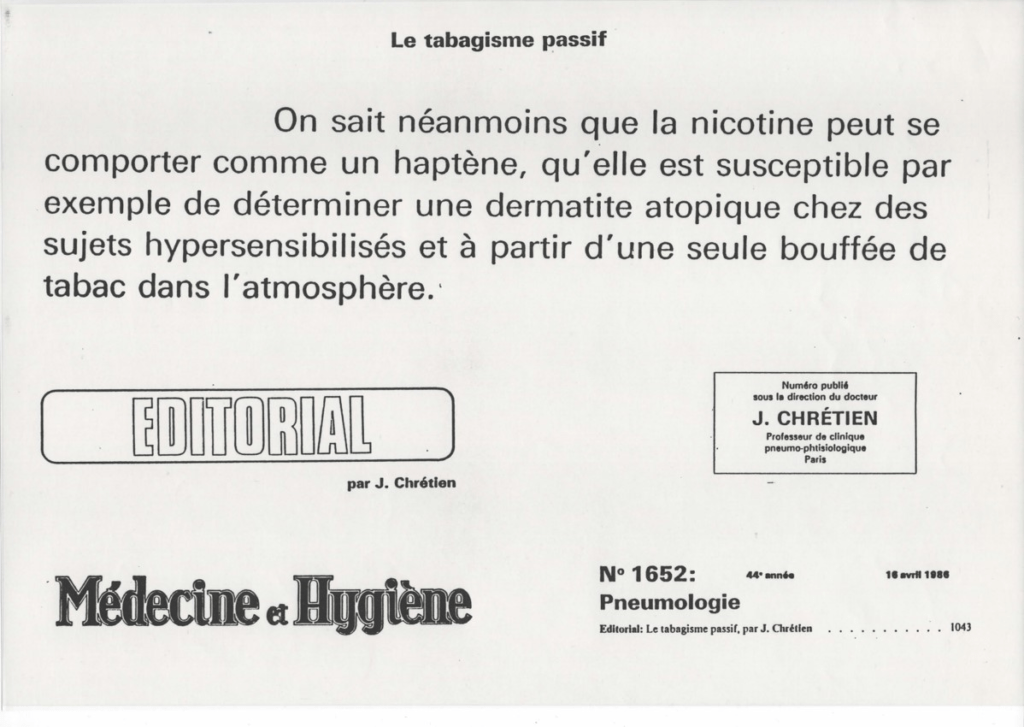
Tobacco allergen and hapten nicotine
So I decided to apply a patch of maceration of cigar leaves on my left forearm. After 15 minutes, the reaction was intense and urticarial with a reaction to the face. The same solution was negative in a lab colleague. A doctor I knew gave me an intradermal test the following week with allergenic tobacco extracts from the Institut Pasteur at 1/100,000. The response was very positive after 15 minutes with also a reaction to the face.
We then initiated a specific desensitization with allergenic tobacco extracts and a certain success despite the variability of allergenic extracts that I tried to standardize with the École Nationale Supérieure de Chimie de Mulhouse (6).
Assistance from several international laboratories
Degranulation of human basophils (Paris, France)
In 1977, I contacted researcher Jacques Benveniste, director of research at INSERM who had developed the deganulation test for human basophils (Baso-Kit, Mérieux) in correlation with the detection of specific IgE. I published a second paper in 1979 (7).
Passive cutaneous anaphylaxis (Bern, Switzerland)
At the same time, I contacted Alain de Weck from the Institute of Clinical Immunology in Bern (Switzerland), who suggested that I gather my family’s serums in order to check passive positive skin anaphylaxis in rabbits and guinea pigs in his department. The results were positive with tobacco and nicotine. While my manuscript was in press in the Revue Française d’Allergologie, Alain de Weck suggested that I withdraw my paper to publish together. I then refused and was surprised to be published by the editor of Allergie et Immunologie in Paris to whom I had sent my paper for information. The Revue Française d’Allergologie cancelled my publication because my paper was no longer original.
After these events, I took the opportunity to inform the British Medical Journal about the harmful role of passive tobacco smoke for skin diseases while stating that the results of Alain de Weck would be published soon (8).
Tobacco specific IgE (New Orleans, USA)
I also sent the serums of my family to Samuel B. Lehrer (Tulane University, New Orleans, USA) to determine the specific IgE with the tobacco allergen (9). I then had a specific RAST (RadioAllergoSorbent Test) IgE tobacco class 4 while the other members of my family were negative, showing the highest sensitivity of the Benveniste test directly with the basophils of each patient.
A cream of sodium cromoglycate
I then successfully developed a sodium cromoglycate cream to stabilize the tissue mast cells at the base of the sebaceous glands (10). The pharmaceutical industry in Basel did not follow up on the development of this cream because anti-leukotrienes were being developed. Competition for local corticosteroids was certainly also an unavowed cause.
I then published in many Anglo-Saxon journals the potential allergic origin of seborrheic dermatitis (11,12,13).
The seborrhea dogma collapses
A 1983 publication showed that the rate of seborrhea was the same in two groups of patients with or without seborrheic dermatitis (14) thus negating the existing dogma.
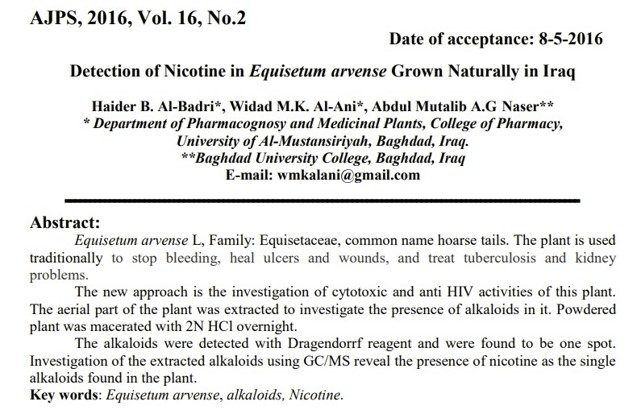
Nicotine in horsetails
I had the opportunity to directly check my allergic reactions by innocently pulling horsetail from my right hand in front of my house with an arm and face reaction. After verification, horsetail (Equisetum arvense L.) contains nicotine (15). I had the same reaction with my second brother by weeding sedums during our school holidays. A 1945 publication confirmed the presence of nicotine in this plant (16).

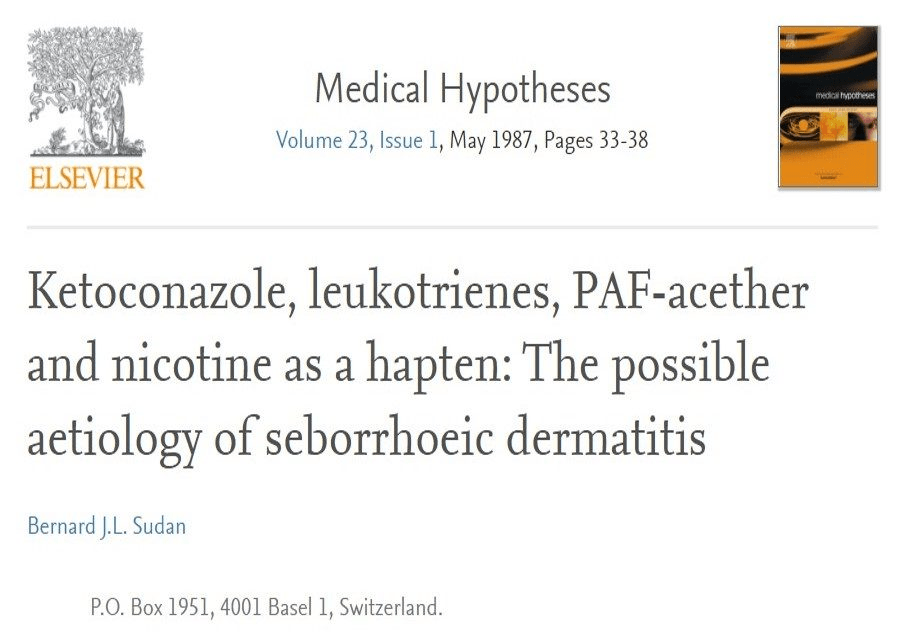
Ketoconazole, anti-leukotriene
After my first publications that undermined the fragile involvement of the sebaceous glands, I was surprised to find that ketoconazole, an anti-fungal molecule used to treat seborrheic dermatitis, also had anti-leukotrienes properties therefore anti-allergic (17,18).

Pityrosporum, saprophyte of the skin
In the meantime, dermatologists were trying to emphasize the involvement of the Pityrosporum fungus by specifically describing seborrheic dermatitis as pityrosporosis (19) while citing my family allergy to nicotine. At the end of their publication in an addendum, these authors cited research that showed that lithium succinate, a lithium salt (Lithioderm©) had no activity against pityrosporum.
Indeed, the involvement of Pityrosporum, a skin saprophyte present on all inflamed skin does not hold because solutions based on lithium succinate, lithium salt have no activity (20) against this fungus showing that the origin of seborrheic dermatitis is definitely allergic.
Chewing gum, patches and nicotine vaccines
Several publications have reported allergic reactions after chewing gum and nicotine patches with my responses to editors (21, 22, 23).
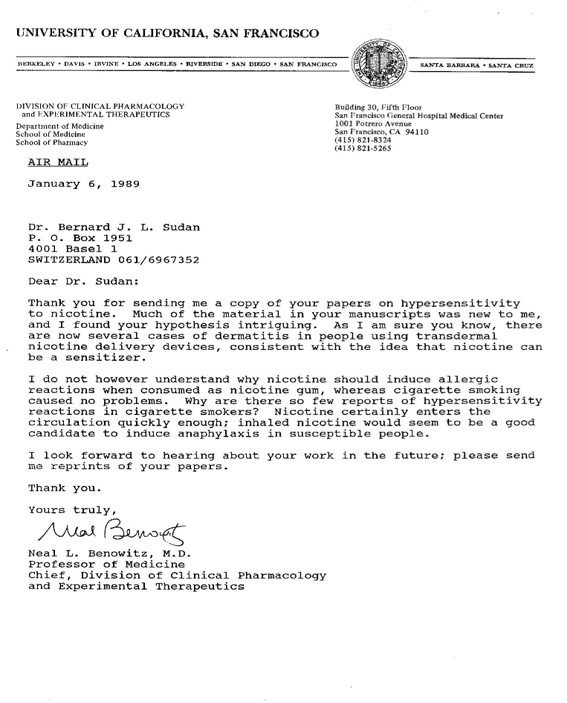
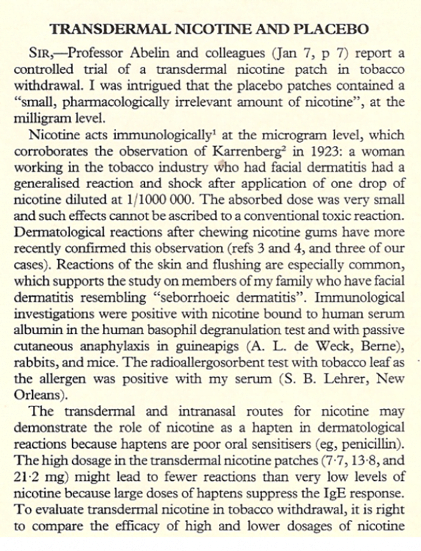
Then I refuted a study by the famous British magazine The Lancet in early 1989. The authors wanted to minimize the dermatological side effects of nicotine patches (7.7 mg, 13.8 mg and 21.2 mg of nicotine) by comparing them with a placebo that contained 1 mg of nicotine (24). I told the editor that a placebo had to be neutral and he published immediately.
In addition, the development of a nicotine vaccine was discontinued following several cases of anaphylactic shock (25) including one of the following descriptions: “One subject in the Phase IIb trial of NicVAX vaccine had an anaphylactic allergic reaction that resolved with medication.”
The immunology of nicotine
Professor Ronald R. Watson (USA) immediately asked me to publish a chapter on nicotine immunology (26) in his book.
The slow confirmations
In 1998, researchers published a confirmation of my work on hapten nicotine without quoting me (27). After a nicotine-positive intradermal test in a hypersensitive patient, they applied a nicotine patch that caused generalized hives.
It took another 20 years in 2018 to randomly test a patient with seborrheic dermatitis with nicotine. The authors are also amnesic about my original works of 1978 (28).
Histamine in the skin
Researchers linked the presence of histamine in the skin of seborrheic dermatitis related to itching in 2011 (29), also supporting my theory and allergic research with the involvement of tissue mastocytes.
Allergies, smoking and seborrheic dermatitis
Recently, a Russian publication has observed the link between allergies and seborrheic dermatitis (30).
Another Indonesian publication noted a link between smoking and seborrheic dermatitis (31).
Solution to Dead Sea Salts
After observing the effectiveness of sodium cromoglycate in 1980, I also noticed the beneficial effect of seawater, which reminded me of the work of biologist René Quinton.
I have linked effective molecules such as sodium cromoglycate, lithium succinate, lithium salt and seawater. So in early 2010, I had the opportunity to test a dermatological soap based on Dead Sea salts as well as a moisturizer of the same brand to see a great effectiveness with the confirmation of a large number of people with seborrheic dermatitis, psoriasis or atopic dermatitis.
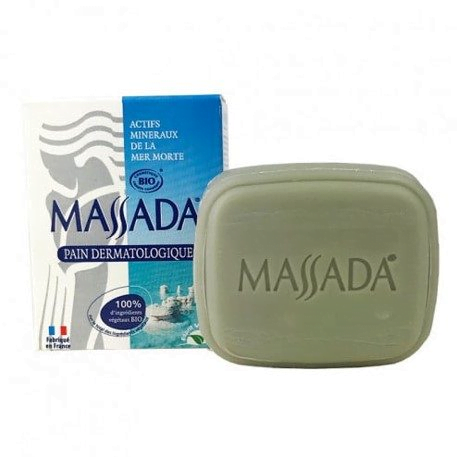

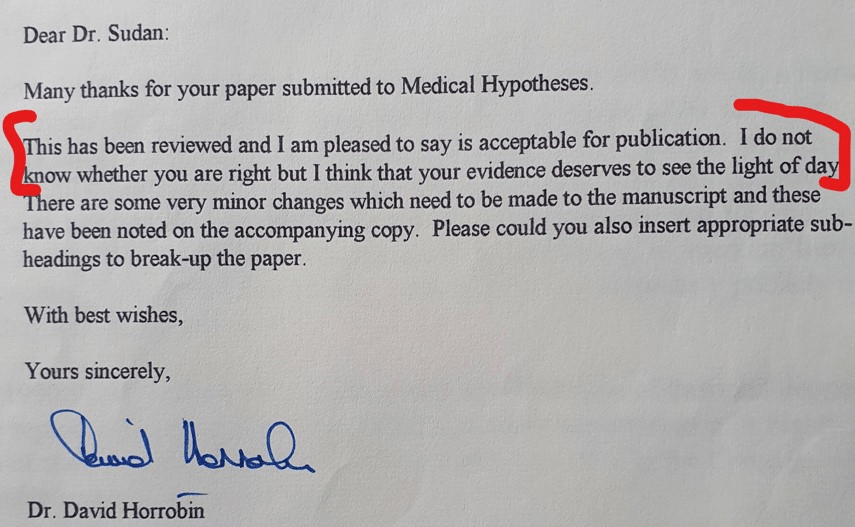
Medical hypotheses without medical hypotheses
I summarized my results in a manuscript accepted at first in Medical Hypotheses and then refused with the false pretence that this efficacy was known (32, 33). Looking carefully at the PubMed scientific database, I found no publication describing the beneficial effects of Dead Sea salts for seborrheic dermatitis. Once again, I would like to thank the founder and first editor of Medical Hypotheses, David Horrobin, for publishing me four papers showing his open-mindedness in fostering the development of medical hypotheses.
Mast cells at the base of sebaceous glands
A recent publication (34) shows the crucial role of mast cells at the base of the sebaceous glands for both seborrheic dermatitis and atopic dermatitis.
My paper and digital book
https://www.lulu.com/spotlight/bjls
My blog
I summarize all my work on my blog as well as the published work on the theme of skin diseases and especially so-called seborrheic and atopic dermatitis as well as psoriasis.
Bernard SUDAN
April 2023
References:
(*) It is not necessary to repeat that neither AIMSIB nor any of its members received any subsidy from the manufacturers of cream enriched with sodium cromoglycate, lithium succinate, lithium salt, or seawater.
- Sudan BJL. : Contribution à l’étude du rôle allergénique de fumée de tabac. Le tabac : un allergène, la nicotine: un haptène, Allergie et Immunologie 1978;10:36-54.
- https://bernardsudan.net/historique-de-mes-travaux-depuis-1978-letiologie-de-ma-dermatite-seborrheique-familiale-avec-lhaptene-nicotine-et-les-sels-de-la-mer-morte/
- Unna PG. : Das seborrheische Ekzem. Monatsheft für praktische Dermatologie 1887; 6:827-846. https://archive.org/details/b22302438
- Pringle JJ : Rare seborrhoide of face. British Journal Dermatology, 1903, 41-47. https://www.deepdyve.com/lp/wiley/a-rare-seborrho-de-of-the-face-h7bSAhK0tq
- Karrenberg CL. Zur Kasuistik der phytogenen Berufsdermatosen: Hauterkrankung durch Tabakblätter. Dermatol Z. 1928; 52:30–9. https://www.karger.com/Article/Abstract/252158
- Sudan BJL, Brouillard C, Strehler C, Strub H, Sterboul J, Sainte-Laudy J. : Determination of nicotine in allergenic extracts of tobacco leaves by high-performance liquid chromatography. Journal of Chromatography, 1984, 288, 415-422. https://www.sciencedirect.com/science/article/abs/pii/S0021967301937173
- Sudan BJL, Sterboul J. : Sensibilisation tabagique. Le tabac : un allergène, la nicotine: un haptène. Diagnostic par le test de dégranulation des basophiles humains. Nouv. Presse Méd. 1979;8:356. https://api.semanticscholar.org/CorpusID:80416406
- Sudan BJL: Breathing other people’s smoke. British Medical Journal, 2, 895, 1978. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1608474/
- Sudan BJL: Tobacco smoke sensitivity: a result of allergy? Annals of Allergy, 1987, 23, 223-224. https://europepmc.org/article/MED/3826774
- Sudan BJL, Sterboul J: Dermite séborrhéique et cromoglycate de sodium. Cutis (Paris), 1980, 4, 81-85.
- Sudan BJL, Sterboul J. Nicotine : an hapten. Brit. J. Dermatol. 1981;104:349-50. https://academic.oup.com/bjd/article-abstract/104/3/349/6688405?redirectedFrom=fulltext
- Sudan BJL: Passive smoking: nicotine, a hapten. Food and Chemical Toxicology, 20, 629, 1982. https://www.sciencedirect.com/science/article/abs/pii/S0278691582900023?via%3Dihub
- Nicotine as a hapten in seborrhoeic dermatitis. Contact Dermatitis 1984; 11:196-7. https://onlinelibrary.wiley.com/doi/10.1111/j.1600-0536.1984.tb00979.x
- Burton JL, Pye RJ. Seborrhea is not a feature of seborrheic dermatitis. British Medical Journal, 1983, 286: 1169-1170. https://www.bmj.com/content/286/6372/1169
- Sudan BJL. Seborrhoeic dermatitis induced by nicotine of horsetails (Equisetum arvense L.). Contact Dermatitis 1985; 13:201-2. https://onlinelibrary.wiley.com/doi/10.1111/j.1600-0536.1985.tb02548.x
- Marion L. The alkaloids of Sedum acre. Canadian Journal of Research, 1945, 23b, 5. https://cdnsciencepub.com/doi/abs/10.1139/cjr45b-020
- Beetens JR, Loots W, Somers Y, Coene MC and de Clerck F. Ketoconazole inhibits the biosynthesis of leukotrienes in vitro and in vivo. Biochemical Pharmacology, 1986, 35, 883-891. https://www.sciencedirect.com/science/article/abs/pii/0006295286900729?via%3Dihub
- Sudan BJL. : Ketoconazole, leukotrienes, PAF-acether and nicotine as a hapten : the possible aetiology of seborrheic dermatitis. Med. Hypotheses 1987; 23:33-38. https://www.sciencedirect.com/science/article/abs/pii/0306987787901770?via%3Dihub
- Grosshans E., Bressieux A.: L’eczéma séborrhéique (La pityrosporose), Annales de Dermatologie et de Vénéréologie, 1988, 115, 79-86. https://europepmc.org/article/MED/2967043
- Boyle J, Burton JL, Faergemann J. Use of topical lithium succinate for seborrhoeic dermatitis. British Medical Journal,1986; 292:28. https://www.bmj.com/content/292/6512/28.1
- Sudan BJL : Rash from nicotine gum : Nicotine as a hapten. Southern Medical Journal, 1988, 81, 287. https://europepmc.org/article/MED/3340887
- Sudan BJL. Niacin, Nicotine and Flushing. Annals of Pharmacotherapy, 1994, 28, 113. https://journals.sagepub.com/doi/abs/10.1177/106002809402800925.
- Sudan BJL. Nicotine TTS-Systems and Adverse Reactions : Skin Irritation, Skin Sensitization and Nicotine as a Hapten. Journal of Clinical Psychopharmacology, 1995, 15, 145-146. https://scholars.duke.edu/display/pub752454
- Sudan BJL. Transdermal nicotine and placebo. The Lancet 1989; 1:334. https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(89)91350-0/fulltext
- Gorelick DA. Pharmacokinetic approaches to treatment of drug addiction. Expert Rev Clin Pharmacol 2008;1:277-90. https://www.tandfonline.com/doi/full/10.1586/17512433.1.2.277
- Sudan BJL, Sainte-Laudy J. Nicotine and Immunology. In: Drugs of Abuse and Immune Function. Watson RR ed., CRC Press; 1990. p.113-23. https://books.google.fr/books?id=5ePEDE1-r5YC&pg=PA113&lpg=PA113&dq=nicotine+and+immunology+sudan+bernard&source=bl&ots=_K99KFJQRH&sig=ACfU3U0vC8nYtHelCk1pl3Dh7q5I-76yfg&hl=fr&sa=X&ved=2ahUKEwihlY7_hsntAhWry4UKHQBvDHcQ6AEwBXoECAcQAg#v=onepage&q=nicotine%20and%20immunology%20sudan%20bernard&f=false
- Lee IW, Ahn SK, Choi EH, Lee SH, Urticarial reaction following the inhalation of nicotine in tobacco smoke, British Journal of Dermatology, 1998, 138, 3, 486–488. https://academic.oup.com/bjd/article-abstract/138/3/486/6682954?redirectedFrom=fulltext
- Susic Alen, Klepo L, Islamagic E, Ostogic J., Suljevic D. : Nicotine allergy in correlation with different sources and individual predispositions, Albanian Medial Journal, 2018, 1, 13-19. https://www.researchgate.net/publication/324057693_Nicotine_allergy_in_correlation_with_different_sources_and_individual_predispositions
- Kerr K, Schwartz JR, Filloon T, et al. Scalp stratum corneum histamine levels: novel sampling method reveals association with itch resolution in dandruff/seborrhoeic dermatitis treatment. Acta Derm Venereol. , 2011; 91:404-8. https://medicaljournalssweden.se/actadv/article/view/9085
- Barillo AA, Smirnova SV : Causal relationship between allergy and seborrheic dermatis, Bulletin of Siberian Medicine, 2022, 21, 13-18. https://www.researchgate.net/publication/362114654_Causal_relationship_between_allergy_and_seborrheic_dermatitis
- Ahmad Dista Alkholqui. Thèse : La relation entre le tabagisme et la dermatite séborrhéique chez les adultes âgés de 30 à 60 ans (Indonésie) Universitas Trisakti, Djakarta, 2022.
- Sudan B. Dead sea salts as a new approach for the treatment of seborrheic dermatitis. Le Blog de Bernard Sudan, 22 juillet 2021. https://bernardsudan.net/dead-sea-salts-as-a-new-approach-for-the-treatment-of-seborrheic-dermatitis/
- Sudan B. Les sels de la Mer Morte comme nouvelle approche pour le traitement de la dermite séborrhéique. Le Blog de Bernard Sudan, 22 juillet 2021. https://bernardsudan.net/les-sels-de-la-mer-morte-comme-nouvelle-approche-pour-le-traitement-de-la-dermatite-seborrheique/
- Shree Harsha Vijaya Chandra, Ramasamy Srinivas, Thomas L Dawson Jr , John E Common . Cutaneous Malassezia: Commensal, Pathogen, or Protector? Front Cell Infect. Microbiol., 2021, 10. https://www.frontiersin.org/articles/10.3389/fcimb.2020.614446/full
Ex Chef de laboratoire en toxicologie et pharmacologie LabHead Ciba-Geigy, CIBA, Novartis, Bâle, 1975-2006 Research Nicotine as a hapten in seborrheic dermatitis, The Lancet, British Medical Journal, British Journal of Dermatology, Food and Chemical Toxicology, « Nicotine and Immunology » in Drugs of Abuse and Immune Function Ronald R. Watson ed.
https://www.researchgate.net/profile/Bernard-Sudan
https://www.dermiteseborrheique.net
https://www.bernardsudan.net/
https://www.youtube.com/channel/UCeQB3vdsKeZU-E0zORZr0vQ?view_as=subscriber